Obsessive-compulsive disorder often goes underdiagnosed and undertreated, resulting in psychological distress, social dysfunction, and diminished quality of life. On this page, learn how to access the necessary mental health treatment with your United Healthcare Insurance, how The Sylvia Brafman Mental Health Center can restore your emotional well-being, and answers to the common question: “What does UHC cover for OCD?”

Obsessive-Compulsive Disorder (OCD) Therapy and Treatment in Florida with United Healthcare
What are the Common Symptoms of Obsessive-Compulsive Disorder (OCD)?
Obsessive-compulsive disorder (OCD) is a mental health condition that can severely impact daily life. People with OCD experience persistent, intrusive thoughts called obsessions that cause intense anxiety and psychological distress. To cope with these obsessions, individuals may engage in compulsive behaviors that involve repetitive actions aimed at reducing the anxiety caused by the obsessions.

Who is United Healthcare?
UnitedHealthcare (UHC), founded in 1977, is a leading health insurance provider in the United States. With a mission to improve the healthcare system’s efficiency and affordability, UHC offers a wide range of health plans and services. As part of the larger UnitedHealth Group, the company is committed to enhancing healthcare access and outcomes for individuals and communities.
Based in Minnesota, United Healthcare plans include individual, family, group, Medicare Advantage, Medicare Supplement, and Medicaid community options. The company enhances member experiences with United Healthcare wellness programs, a nurse hotline, and online tools, while the United Healthcare member portal and mobile app facilitate easy account management, claims, and access to educational resources. The United Healthcare network comprises doctors, hospitals, specialists, and pharmacies, providing flexibility to choose between in-network and out-of-network providers.

Do United Healthcare Insurance Policies Cover Mental Health Treatment?
Yes. The network of United Healthcare providers includes facilities and specialized clinicians for the treatment of mental health and substance use problems. These benefits are available within plans offering behavioral health services. To verify the details of your plan’s behavioral health benefits, including coverage levels and any applicable limitations or exclusions, please consult your policy documents or call 877-958-9212.
Mental health treatment and services are recognized as an essential component of comprehensive healthcare, and United Healthcare aims to support its members in accessing necessary care. Coverage may include Cognitive Behavioral Therapy (CBT) sessions, supportive counseling, psychiatric evaluations, and, in some cases, hospitalization for mental health-related issues.
Does United Healthcare Cover OCD Treatment in Florida?
Yes, UHC typically covers OCD treatment in Florida. Treatment often involves a blend of therapeutic interventions, including Acceptance and Commitment Therapy (ACT) sessions, telehealth, medications, and peer support for OCD. Whether for yourself or a loved one, these resources can assist in managing and overcoming the condition.
Examine the specifics of your plan to understand coverage details, such as in-network providers, copayments, deductibles, and any prior authorization requirements. For clarity on coverage and to explore available resources for OCD treatment, call 877-958-9212. Our team can provide valuable assistance navigating your UHC insurance plan and obtaining the necessary information for your mental health care needs.
At The Sylvia Brafman Mental Health Treatment Center in Fort Lauderdale, Florida, our team of dedicated professionals is ready to guide you. We offer IOP and a variety of treatments programs, each uniquely designed to meet your needs. So don’t wait, reach out to us today! Either give us a call or fill up the form below to request a callback.
"*" indicates required fields

Does United Healthcare Cover Therapy and Counseling for Obsessive-Compulsive Disorder in Florida?
If you’re in Florida and seeking coverage for obsessive-compulsive disorder (OCD), UnitedHealthcare (UHC) offers therapy and counseling for this condition within its behavioral health benefits. The comprehensive health plans that include these benefits ensure the necessary supportive counseling and therapy for OCD. You can maximize these benefits by choosing from in-network providers.
For accurate and current information about “How much does UHC cover for therapy” under your specific plan, review your policy documents or call 877-958-9212. We can provide specifics on what’s covered regarding your treatment needs and any potential out-of-pocket costs associated with these services, including copayments and deductibles.
Does UHC Cover Florida Psychiatrist Visits for OCD Treatment?
United Healthcare (UHC) generally includes coverage for psychiatrists’ use in treating OCD as part of its extensive mental and behavioral health services. This coverage facilitates access to specialized care, encompassing OCD medications and psychiatric evaluations, promoting holistic approaches to OCD. Specifics of coverage vary across plans.
For detailed information about your coverage for psychiatric services related to OCD, call 877-958-9212. The commencement of your emotional well-being is just a phone call away.
Does United Healthcare Cover OCD Medications?
United Healthcare (UHC) typically covers medications prescribed for treating OCD. If you are in need of pharmacological treatment for OCD, you can find comprehensive support within United Healthcare plans. To get the most accurate information, it’s recommended that you review the prescription drug formulary for your specific plan or contact The Sylvia Brafman Mental Health Center at 877-958-9212.
Obsessive-Compulsive Disorder Treatment Programs Covered by UnitedHealthcare
United Healthcare Insurance provides coverage for programs that address obsessive-compulsive disorder (OCD). These programs include therapy, medications, and other support services. To find out more about the OCD programs that UHC generally covers, browse the following sections explaining the therapeutic interventions offered. For details on a program that meets your treatment needs, call 877-958-9212.

Florida OCD Treatment Centers in Florida That Accept United Healthcare Insurance
The Sylvia Brafman Mental Health Center in beautiful sunny Florida is a leading, accredited provider of evidence-based treatment for obsessive-compulsive disorder (OCD). Acknowledging the complexities of managing this condition, we offer personalized treatment options that empower our patients through comprehensive psychotherapy, inpatient and outpatient programs, medication education, and support groups.
For those seeking rehabs in Florida that accept UHC Insurance, our center may take your particular plan. Call 877-958-9212 to learn more about our customized treatment programs for OCD. Our compassionate team is ready to provide the support you need, verify insurance coverage, answer questions, and guide you through the rehab admissions process.
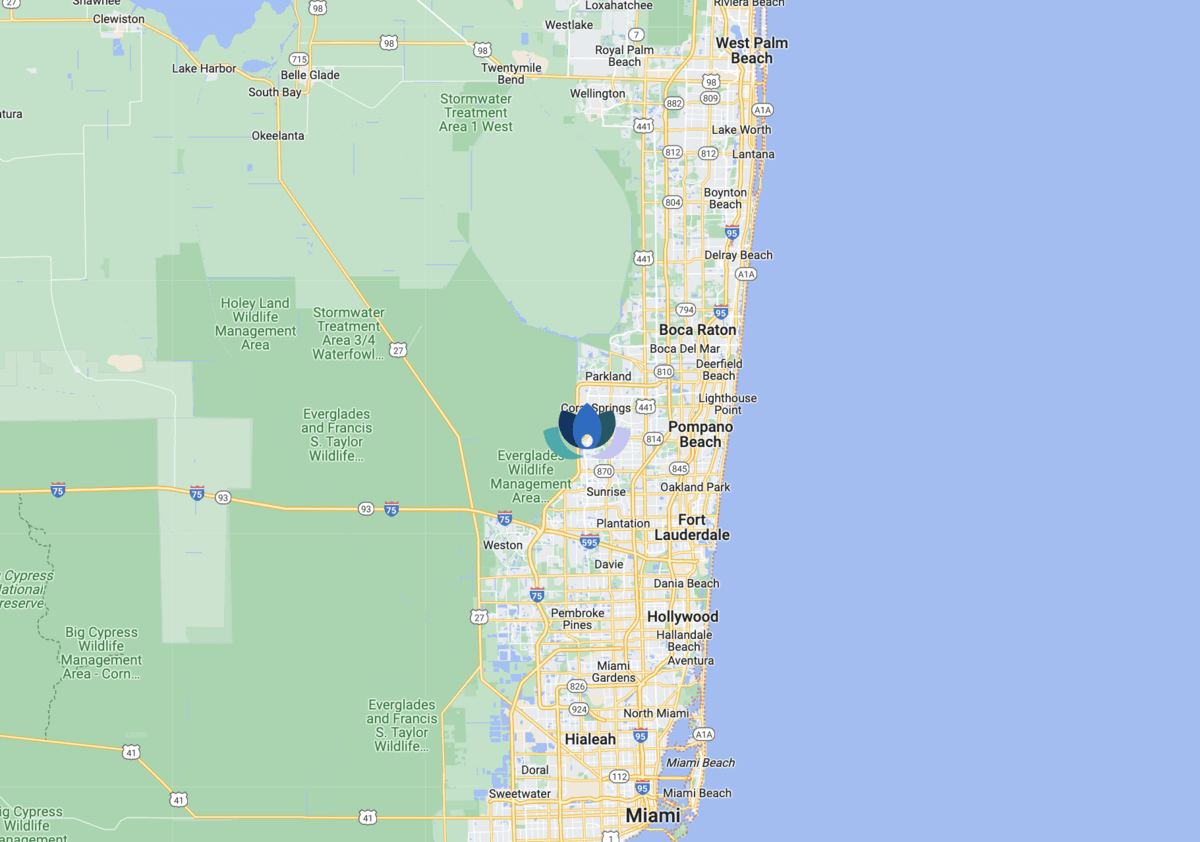
You may also choose to visit our physical location at the address below:
- The Sylvia Brafman Mental Health Center: 7710 NW 71ST CT, Tamarac, Florida, 33321
How Much Does OCD Treatment Cost Without United Healthcare Insurance?
On average, in-person therapy sessions without insurance vary from $100 to $200, while a brand name, one month’s supply of a Selective Serotonin Reuptake Inhibitor (SSRI) for OCD can run anywhere from $43 to almost $300. Factors influencing OCD treatment costs vary, including the provider’s qualifications and therapeutic methods.
Call 877-958-9212 for more accurate cost estimates regarding your specific needs and customized guidance on the appropriate OCD treatment.
How To Check My UHC Health Insurance Policy Coverage Levels
If you’re looking for a free and thorough OCD screening and assessment of your UHC health Insurance plan, we’re here to help. Call 877-958-9212 to speak with our patient advocates at The Sylvia Brafman Mental Health Center. We’re dedicated to assisting you in gaining clarity on your mental health insurance coverage.
Once we’ve verified your insurance information, we’ll guide you through the specifics of your policy. This includes providing detailed information on various treatment options, program selections, and potential out-of-pocket costs. Our main aim is to provide you with the knowledge you need to make well-informed decisions about your mental health treatment so you can develop coping strategies for OCD and improve your emotional well-being. Let us help you navigate the complexities of your coverage so that you can focus on your recovery.



