Are you and your partner seeking mental health therapy? The Sylvia Brafman Mental Health Center in South Florida specializes in treating adults with various mental health disorders. We also accept United Medical Resources (UMR) plans and offer housing options for out-of-state patients. Continue reading to learn how to access couples therapy for mental and emotional wellness with UMR health benefits.

Does United Medical Resources (UMR) Cover Mental Health Therapy for Couples Treatment and Therapists in Florida?
Who is United Medical Resources (UMR), the Health Insurance Provider?
United Medical Resources (UMR) operates as the nation’s largest third-party administrator (TPA), specializing in managing administrative services for self-funded employer-sponsored health plans. As a subsidiary of UnitedHealth Group, one of the largest healthcare services companies in the U.S., UMR third-party administration does not directly sell health insurance policies to individuals or families.
Instead, it collaborates with employers to oversee their self-funded health plans. UMR healthcare management provides comprehensive administrative support, including UMR claims processing, a provider network, member enrollment, and customer service. The UMR provider network comprises healthcare professionals and facilities, ensuring plan members can access diverse medical services. UMR preferred providers help control costs while maintaining quality care standards.
Moreover, UMR wellness programs promote the wellbeing of employers and employees. These initiatives encompass mental health resources, preventive care services, and lifestyle management strategies.

Mental Health Programs with Couples Therapy Covered by Blue Cross Blue Shield Insurance
BCBS of Minnesota prioritizes mental health within its health coverage options. Through various mental health programs and services, the health insurance provider extends support to individuals navigating challenges from depression to substance abuse, emphasizing access to resources for optimal emotional and psychological wellness. Below, we’ve highlighted some mental health couples therapy programs typically covered by BCBSMN.

At The Sylvia Brafman Mental Health Treatment Center in Fort Lauderdale, Florida, our team of dedicated professionals is ready to guide you. We offer IOP and a variety of treatments programs, each uniquely designed to meet your needs. So don’t wait, reach out to us today! Either give us a call or fill up the form below to request a callback.
"*" indicates required fields

What Type of Mental Health Disorders Does UMR Cover for Two People?
The mental health disorders covered by United Medical Resources (UMR) are usually determined by the terms and conditions of your employer’s self-funded health plan. Nonetheless, UMR-administered health plans are typically obligated to provide coverage for a broad spectrum of mental health disorders. Please note that the following isn’t a complete list of all mental health disorders covered by your plan.

Does UMR Cover Therapy and Treatment for Dual Diagnosis for Couples?
Yes, UMR may cover therapy and treatment for couples seeking to manage a dual diagnosis. Dual diagnosis refers to individuals who struggle with both substance use and a mental health disorder simultaneously. UMR’s coverage for such treatment depends on the specific terms and conditions of the employer’s self-funded health plan.
Treatment for dual diagnosis typically involves integrated therapy that addresses both substance abuse and mental health issues at the same time. This can include individual therapy, couples therapy exercises, medication management, and more. Couples therapy benefits for those facing dual diagnosis include improving communication skills, strengthening love and partnership, and providing mutual support during recovery.
Review your UMR health insurance plan details and call 877-958-9212 to schedule a free assessment to determine the most suitable care for you and your partner. We can also provide detailed estimates related to the common question: “How much does UMR cover for therapy?”
Mental Health Therapy and Rehab Centers in Florida That Take UMR Health Insurance
The Sylvia Brafman Mental Health Center prioritizes comprehensive services with a distinct focus on mental health awareness in South Florida. Our experienced team of medical and clinical professionals is dedicated to ensuring accurate diagnoses and effective treatment for all our patients. Over our years of operation, we have aided numerous individuals in overcoming their mental health challenges.
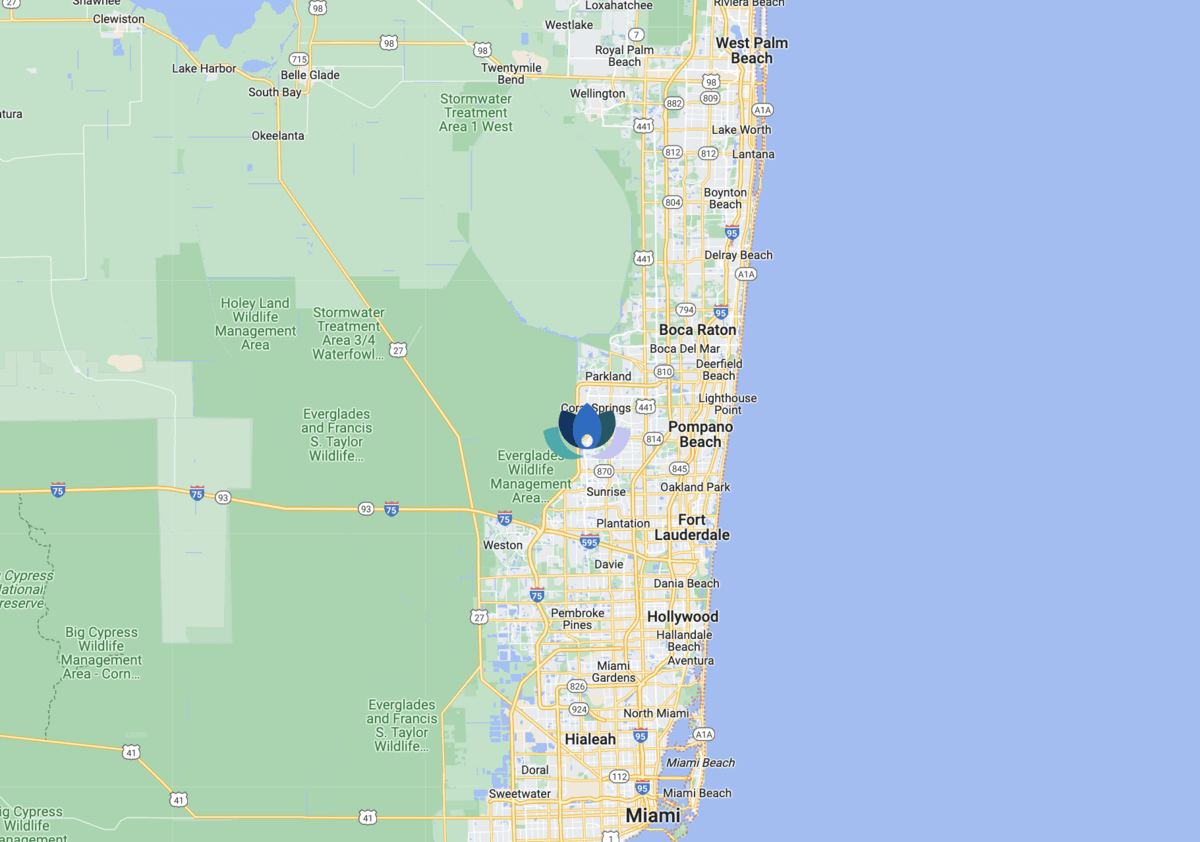
Our mental health center may accept your health insurance policy administered by UMR. To learn more about our couples therapy techniques and your mental health benefits, call 877-958-9212 to speak with a helpful patient advocate. You’re also welcome to visit our treatment facility at the address provided below:
- The Sylvia Brafman Mental Health Center: 7710 NW 71ST CT, Tamarac, Florida, 33321
How Much Does Couples Rehab Cost with UMR Insurance?
Rehabs in Florida that accept UMR-administered health plans will likely result in treatment costs that are partially or fully covered. These expenses vary considerably and are influenced by factors such as the location of the treatment facility, the services provided, and any additional amenities. With insurance, copayments for couples therapy sessions typically range from $10 to $100.
Contact us for detailed information regarding your specific treatment needs and your United Medical Resources-administered insurance policy.
How To Check My UMR Health Insurance Coverage Levels for Two People
To gain insight into the scope of your health insurance coverage, contact us today. Our patient advocates are ready to provide the necessary information. We’ll connect with UMR member services to confirm coverage specifics and thoroughly examine your policy alongside you. Our detailed breakdown of the available treatment and program options for couples therapy can facilitate informed decisions regarding mental healthcare.
How Many Times Will United Medical Resources Pay for Couples Rehab in Florida?
The frequency of United Medical Resources’ coverage for couples rehabilitation hinges on various factors, including your policy’s particulars, the nature of the rehabilitation required, and its medical necessity. UMR typically extends coverage for rehabilitation services when they are deemed medically necessary and fall within the plan’s coverage parameters.
Several key considerations come into play:
- Medical Necessity: Like other healthcare providers, UMR’s coverage decisions revolve around medical necessity. This entails that the treatment must be recommended by a healthcare provider and deemed essential for recovery or wellbeing.
- Type of Rehabilitation: Different criteria and limitations may apply to the coverage of each type of rehabilitation.
- Plan Design: The coverage levels and limits vary across the specific UMR-administered health plans employers offer. While some plans stipulate a predetermined number of covered rehabilitation sessions, others provide coverage as long as it remains medically necessary.
- Prior Authorization: Certain services may necessitate preauthorization or prior approval before coverage kicks in.
- Out-of-Pocket Costs: Despite coverage, individuals may still bear out-of-pocket expenses such as copayments, deductibles, or coinsurance.



