How Much Does BPD Treatment Cost in Florida?
The cost of borderline personality disorder (BPD) treatment in Florida can vary significantly based on several factors, including the type of treatment program, the level of care needed, the location of the healthcare facility, and the specific services provided. Call 877-958-9212 for accurate details regarding BPD treatment costs in Florida.
BPD ranks among the mental health disorders with some of the highest healthcare costs, encompassing both direct and indirect expenses. However, it’s important to note that implementing evidence-based treatment approaches for BPD can enhance your well-being and yield cost-saving benefits when executed effectively.17
Are There Four Stages/Types of BPD?
There are no universally accepted stages or types of borderline personality disorder (BPD), and the progression of symptoms can vary widely from person to person. Some mental health professionals have proposed elegant models of BPD that describe a stage or sub-type based on common patterns of symptoms and behaviors.
For example, Theodore Millon, an expert in personality disorders, puts forth one such model. The four sub-types of BPD, according to his model, are:
Discouraged Borderline: this subtype, which also goes by the name high functioning BPD or quiet BPD, can manifest in several ways in their relationships. While in these relationships, the BPD patient can function quite normally. However, when the relationship ends, their life can crumble. They may also fear the possibility of the end of the relationship, causing strain and, ultimately, a self-fulfilling prophecy. Patients with this subtype of BPD are typically depressed and avoid specific interactions and circumstances. They are often submissive and can be codependent, especially in romantic relationships.
Impulsive Borderline: this subtype of borderline personality disorder often manifests in chaotic behavior not backed by deep thought or reflection. The impulsive borderline’s behavior may cause physical or emotional harm to themselves or others. They are often superficial but charismatic and exciting to be with. Often, these behavior stem from earlier chaos in the family setting where they had to act out to stand out. They may have difficulty dealing with aging, especially if they were praised for their looks or abilities as a child.
Petulant borderline: often manifesting in passive-aggressive behavior, the petulant borderline patient can be seen as pessimistic or negative, impatient, and irritable. Many were insecure and abused emotionally or physically as children, which ultimately left them feeling depressed and inadequate as adults. These patients often experience irrational and overwhelming anger but feel terrible guilt and remorse once they return to baseline.
Self-Destructive Borderline: as the name suggests, self-destructive borderlines often turn their emotions and anger inwards. While they hope to be independent, they are usually submissive and compliant in their relationships. These patients are at a greater risk for self-harm, including suicide.
It is important to note that these stages are not definitive or universally applicable. Some patients will not fall into any subtypes mentioned above, while others may fall into one or more subtypes. Only a proper diagnosis from a qualified mental health professional can effectively address any of the borderline personality disorder subtypes mentioned above.
Bipolar Disorder Versus Borderline Personality Disorder
Bipolar disorder and borderline personality disorder (BPD) are two different mental illnesses that are often confused due to some similarities in symptoms. A borderline personality disorder diagnosis can also be confounded by the fact that most people with BPD suffer from Co-occurring mental illnesses. It is estimated that over 80% suffer from major depressive disorder, and 90% or more have anxiety. This also extends to substance abuse, with a study assessing that 2/3 of those with BPD also abused alcohol, pills, or drugs.
There are some critical differences between these two similar disorders:
- Mood swings: Both disorders involve mood swings, but the patterns and duration of the mood swings can be distinct. In bipolar disorder, mood swings tend to occur in episodes that last for days or weeks, while in BPD, mood swings may occur more frequently and last for shorter periods, even just a few minutes.
- Emotional instability: Both disorders involve emotional instability, but in BPD, emotional instability is typically more intense and can lead to impulsive behavior, anger, and anxiety.
- Impulsivity: Impulsivity is a common symptom of both disorders, but in BPD, impulsivity may be directed towards self-destructive behavior, such as self-harm or substance abuse.
- Self-image: Individuals with BPD often have an unstable sense of self and may struggle with feelings of emptiness or identity disturbance, while individuals with bipolar disorder typically have a stable sense of self.
- Treatment: Bipolar disorder is typically treated with medication, such as mood stabilizers or antipsychotics, while BPD generally is treated with therapy, such as dialectical behavior therapy or schema-focused therapy.
It is important to note that bipolar disorder and BPD can both be serious mental illnesses that require proper diagnosis and treatment from a qualified mental health professional. If you suspect that you or a loved one may be experiencing symptoms of either disorder, it is essential to seek professional help.
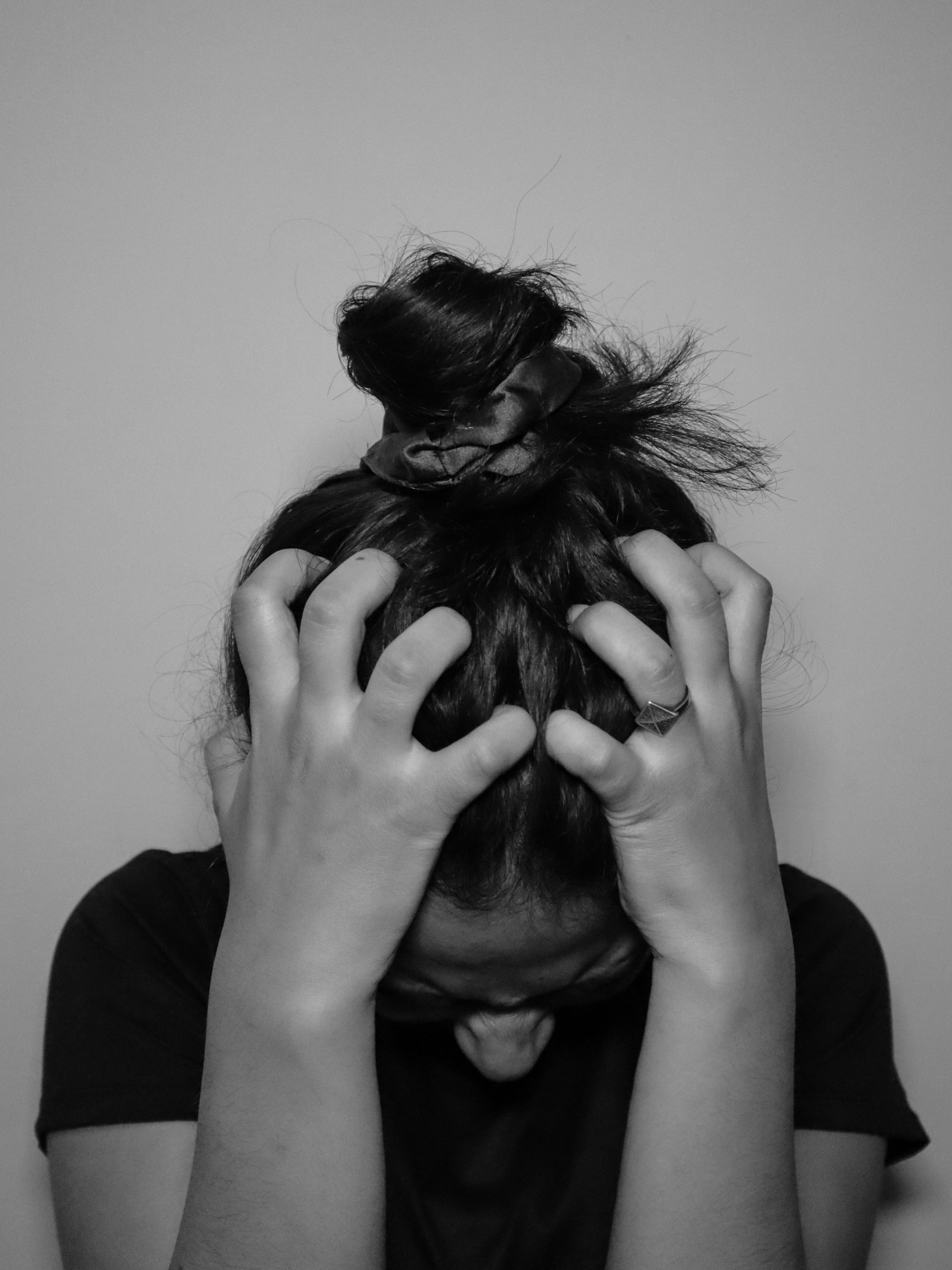
How To Support Your Loved One
If you have a family member or loved one with borderline personality disorder (BPD), you have been suffering just as they have. It can be difficult, to say the least, to set aside the emotional trauma that this disease has caused. However, it’s essential to know that you can help them manage their symptoms and improve their quality of life:
- Educate yourself: Learn as much as you can about BPD. Doing so allows you to better understand your family member’s experience and how to support them. You can start by reading books and articles or attending support groups for families and loved ones of individuals with BPD. This education and understanding of the disease will also help you cope with what will undoubtedly be ups and downs over the coming months and years.
- Encourage professional treatment: Encourage your family member to seek professional help from a qualified mental health professional, such as a therapist or psychiatrist. Offer to help them find a provider, schedule appointments, or accompany them to appointments if needed. You’ve probably tried this before but have not succeeded. If you believe you’ve hit a wall, contact a mental health professional to see if they can assist and intervene.
- Be patient: BPD can cause intense and unpredictable emotions, which can seem impossible for family members to manage. Try to be patient and understanding with your family member, even when their behavior or feelings may be challenging. Remember, this is a disease. They, too, are suffering and don’t want to live this way just as much as you.
- Practice effective communication: Effective communication is vital in maintaining a healthy relationship with any individual, let alone someone with BPD. Use first-person statements to express your thoughts and feelings, listen actively, and avoid blaming or criticizing your family member.
- Establish healthy boundaries: Healthy boundaries protect your well-being. Set limits on what you can do to help and communicate these boundaries clearly without anger or frustration.
Supporting anyone with a mental illness, especially borderline personality disorder, can be very challenging for the caregiver or loved one. Don’t underestimate the effect your loved ones’ disease can have on you; don’t feel that seeing a mental health professional yourself is a sign of weakness. As we say, letting go and admitting that you need help is often the first step toward true healing and long-term mental wellness.
Statistics on Borderline Personality Disorder in Florida
- Prevalence of borderline personality disorder: 1.6% of the general U.S. population (that number may be as high as 5.9%)18
- BPD and self-harm: Approximately 65-80% of individuals with borderline personality disorder engage in some form of non-suicidal self-injury (NSSI).19
- Nearly 75% of BPD diagnoses are given to women, but recent research suggests that borderline personality disorder in men may be comparable. However, men are often misdiagnosed with PTSD or depression.20
- About 70% of individuals diagnosed with BPD will attempt suicide at least once in their lifetime.21
- In a recent study, over 40% of BPD patients were previously misdiagnosed with other disorders, like bipolar disorder.22
- Approximately 10% of people diagnosed with BPD will tragically die by suicide.23
- BPD and comorbidity are common. Other disorders, such as depression, substance abuse, and eating disorders, often co-occur with BPD, making diagnosis and treatment more challenging.24
- Up to 40% of individuals with BPD may also exhibit traits of narcissistic personality disorder.25
- Most individuals with BPD experience a reduction in symptoms as they age, and with proper treatment, they can learn to manage and improve their quality of life.26
- 88% of people with BPD also have anxiety disorders.27
- Borderline personality disorder in women of thirty years old typically has the medical profile of a sixty-year-old woman.28
- Heritability of BPD is estimated to be around 68%.
- Individuals with BPD were significantly more likely to use most types of psychiatric treatments compared to those with major depression.29
- Only a small proportion of those coping with BPD seek psychiatric or psychological care.30
Sources
Sources:
- “Borderline Personality Disorder – Symptoms and Causes – Mayo Clinic.” Mayo Clinic, 13 Dec. 2022, www.mayoclinic.org/diseases-conditions/borderline-personality-disorder/symptoms-causes/syc-20370237.
- “Borderline Personality Disorder.” National Institute of Mental Health (NIMH), www.nimh.nih.gov/health/topics/borderline-personality-disorder. Accessed 31 Oct. 2023.
- Lawrence, Katherine, et al. “Impulsivity in Borderline Personality Disorder: Reward-Based Decision-Making and Its Relationship to Emotional Distress.” Journal of Personality Disorders, vol. 24, no. 6, Guilford Press, Dec. 2010, pp. 785–99. https://doi.org/10.1521/pedi.2010.24.6.785.
- Cuncic, Arlin, MA. “What Is Quiet Borderline Personality Disorder?” Verywell Mind, 8 Nov. 2022, www.verywellmind.com/what-is-quiet-borderline-personality-disorder-5115074.
- Pugle, Michelle. “The Four Types of BPD: Borderline Personality Disorder Can Look Different Depending on the Type.” Verywell Health, 1 Sept. 2022, www.verywellhealth.com/types-of-bpd-5193843.
- Duică, Lavinia, et al. “Borderline Personality Disorder ‘Discouraged Type’: A Case Report.” Medicina-lithuania, vol. 58, no. 2, Multidisciplinary Digital Publishing Institute, Jan. 2022, p. 162. https://doi.org/10.3390/medicina58020162.
- Sussex Publishers, LLC. “Borderline Personality Disorder.” Psychology Today, www.psychologytoday.com/us/basics/borderline-personality-disorder. Accessed 31 Oct. 2023.
- Turvey, Brent E. “Sexual Deviance.” Criminal Profiling, 5th ed., 2023, https://doi.org/10.1016/b978-0-12-385243-4.00008-3.
- “Marsha Linehan | Behavioral Research and Therapy Clinics.” University of Washington, depts.washington.edu/uwbrtc/our-team/marsha-linehan. Accessed 1 Nov. 2023.
- May, Jennifer M., et al. “Dialectical Behavior Therapy as Treatment for Borderline Personality Disorder.” The Mental Health Clinician, vol. 6, no. 2, Mar. 2016, pp. 62–67. https://doi.org/10.9740/mhc.2016.03.62.
- Matusiewicz, Alexis K., et al. “The Effectiveness of Cognitive Behavioral Therapy for Personality Disorders.” Psychiatric Clinics of North America, vol. 33, no. 3, Elsevier BV, Sept. 2010, pp. 657–85. https://doi.org/10.1016/j.psc.2010.04.007.
- Matusiewicz, Alexis K., et al. “The Effectiveness of Cognitive Behavioral Therapy for Personality Disorders.” Psychiatric Clinics of North America, vol. 33, no. 3, Elsevier BV, Sept. 2010, pp. 657–85. https://doi.org/10.1016/j.psc.2010.04.007.
- “A Guide to Transference-Focused Psychotherapy.” McLean Hospital, 11 Feb. 2022, www.mcleanhospital.org/essential/tfp.
- Morgan, Theresa A., and Rawya M. Al-Jabari. “Using Acceptance and Commitment Therapy in the Treatment of Borderline Personality Disorder: Rationale, Preliminary Evidence, and Future Directions.” Current Treatment Options in Psychiatry, vol. 6, no. 4, Springer Science+Business Media, Oct. 2019, pp. 271–83. https://doi.org/10.1007/s40501-019-00185-9.
- Ducasse, Déborah, M. D., and Véronique Brand-Arpon M. A. “Buddhist-Derived Psychotherapies for Borderline Personality Disorder.” National Alliance on Mental Illness (NAMI), 20 Aug. 2021, www.nami.org/Blogs/NAMI-Blog/August-2021/Buddhist-Derived-Psychotherapies-for-Borderline-Personality-Disorder.
- Haslam, Rowan, et al. “A Systematic Review of Scientific Studies on the Effects of Music in People With Personality Disorders.” International Journal of Environmental Research and Public Health, vol. 19, no. 23, Multidisciplinary Digital Publishing Institute, Nov. 2022, p. 15434. https://doi.org/10.3390/ijerph192315434.
- Meuldijk, Denise, et al. “The Value of Psychological Treatment for Borderline Personality Disorder: Systematic Review and Cost Offset Analysis of Economic Evaluations.” PLOS ONE, vol. 12, no. 3, Public Library of Science, Mar. 2017, p. e0171592. https://doi.org/10.1371/journal.pone.0171592.
- “Facts About Borderline Personality Disorder (BPD).” ADAMHS Board of Cuyahoga County, www.adamhscc.org/resources/facts-about-mental-illness/borderline-personality-disorder. Accessed 1 Nov. 2023.
- Chapman, Jennifer. “Borderline Personality Disorder.” StatPearls – NCBI Bookshelf, 2 June 2023, www.ncbi.nlm.nih.gov/books/NBK430883.
- Brickman, Lauren J., et al. “The Relationship Between Non-suicidal Self-injury and Borderline Personality Disorder Symptoms in a College Sample.” Borderline Personality Disorder and Emotion Dysregulation, vol. 1, no. 1, BioMed Central, Aug. 2014, https://doi.org/10.1186/2051-6673-1-14.
- “Borderline Personality Disorder.” NAMI: National Alliance on Mental Illness, www.nami.org/About-Mental-Illness/Mental-Health-Conditions/Borderline-Personality-Disorder. Accessed 1 Nov. 2023.
- Wedig, M. M., et al. “Predictors of Suicide Attempts in Patients with Borderline Personality Disorder over 16 Years of Prospective Follow-Up.” Psychological Medicine, vol. 42, no. 11, 2012, pp. 2395–2404., doi:10.1017/S0033291712000517.
- Ruggero, Camilo J., et al. “Borderline Personality Disorder and the Misdiagnosis of Bipolar Disorder.” Journal of Psychiatric Research, vol. 44, no. 6, Elsevier BV, Apr. 2010, pp. 405–08. https://doi.org/10.1016/j.jpsychires.2009.09.011.
- Paris, Joel. “Suicidality in Borderline Personality Disorder.” Medicina-lithuania, vol. 55, no. 6, Multidisciplinary Digital Publishing Institute, May 2019, p. 223. https://doi.org/10.3390/medicina55060223.
- “Borderline Personality Disorder (BPD).” Mental Health America, mhanational.org/conditions/borderline-personality-disorder. Accessed 1 Nov. 2023.
- Grant, Bridget F. “Prevalence, Correlates, Disability, and Comorbidity of DSM-IV Borderline Personality Disorder: Results From the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions.” Psychiatrist.com, 4 Feb. 2021, www.psychiatrist.com/jcp/prevalence-correlates-disability-comorbidity-dsm-iv-borderline-personality-disorder-wave-2-nesarc.
- “Borderline Personality Disorder (BPD).” Cleveland Clinic, my.clevelandclinic.org/health/diseases/9762-borderline-personality-disorder-bpd#outlook-prognosis. Accessed 1 Nov. 2023.
- “Borderline Personality Disorder (BPD).” Cleveland Clinic, my.clevelandclinic.org/health/diseases/9762-borderline-personality-disorder-bpd#diagnosis-and-tests. Accessed 1 Nov. 2023.
- “BPD Fact Sheet.” National Education Alliance for Borderline Personality Disorder, 29 June 2022, www.borderlinepersonalitydisorder.org/what-is-bpd/bpd-fact-sheet.
- Bender, Donna S., et al. “Treatment Utilization by Patients With Personality Disorders.” American Journal of Psychiatry, vol. 158, no. 2, American Psychiatric Association, Feb. 2001, pp. 295–302. https://doi.org/10.1176/appi.ajp.158.2.295.
- Selby, Edward A., and R. Kathryn McHugh. “Borderline Personality Disorder Symptoms and Treatment Seeking Over the Past 12 Months.” The Journal of Clinical Psychiatry, vol. 74, no. 10, Physicians Postgraduate Press, Inc., Oct. 2013, pp. 1026–28. https://doi.org/10.4088/jcp.12l08232.