At The Sylvia Brafman Mental Health Center, individuals can access comprehensive crisis stabilization programs and services. Our treatment center is committed to providing immediate support and mental health crisis intervention for those in need of acute psychiatric treatment related to issues such as severe mood disturbances, suicidal ideation, or psychotic episodes.
Our crisis response program offers a safe, supportive environment for receiving intensive care from a multidisciplinary team of mental health professionals. Our goal is to stabilize individuals’ conditions, alleviate distressing symptoms, and facilitate a smooth transition to ongoing treatment and support.
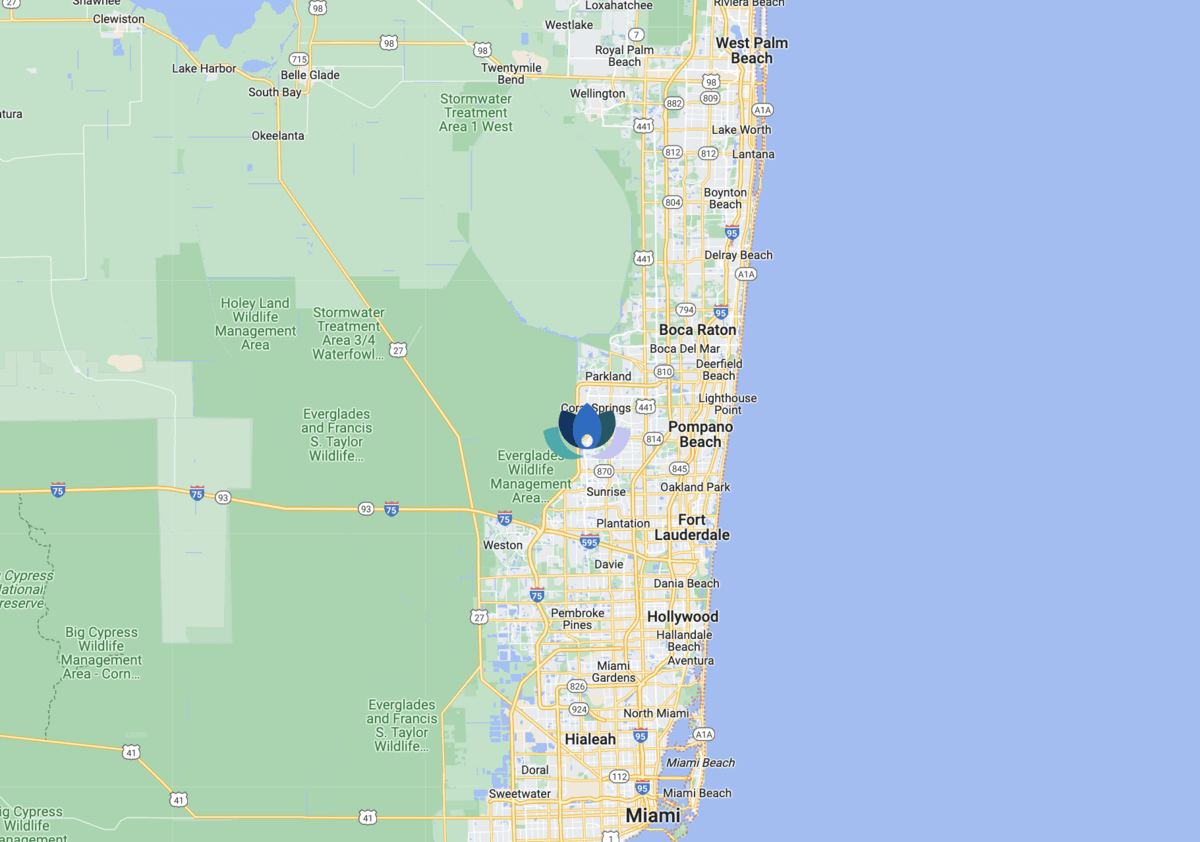
Additionally, The Sylvia Brafman Mental Health Center understands the financial concerns when seeking mental health treatment. Therefore, we accept insurance to help alleviate some of the financial burdens of crisis management services. Our dedicated team of patient advocates works with insurance providers to ensure individuals receive the necessary care while maximizing their mental health insurance coverage. By accepting insurance, we aim to make our top-rated services accessible to those needing emergency psychiatric care and support in South Florida. Please contact our mental health crisis hotline below.