What is the Baker Act and does insurance cover it? This page concisely overviews the Baker Act Florida implemented in 1972. You’ll learn about the criteria for involuntary admission to mental health examinations at psychiatric facilities and key aspects of the process. You will gain essential knowledge about Florida mental health laws and guidelines, as well as whether or not insurance will cover the baker act.

Does Insurance Cover The Baker Act in Florida? | Baker Act Statute, Criteria, and Coverage Details
What Does the Baker Act Mean?
The Baker Act, officially known as the Florida Mental Health Act, allows for involuntary mental health treatment and examination and, if necessary, temporary detention of individuals who may need psychiatric crisis intervention. This law protects individuals who are dangerous to themselves or others, ensuring they receive prompt and appropriate care.
The Baker Act provides a legal means for mental health professionals, law enforcement, and judges to intervene when someone is unable or unwilling to seek help voluntarily. Understanding this Florida mental health law is crucial for anyone concerned about the mental well-being of themselves or others.
Under the Baker Act, an individual may be transported to a receiving facility for involuntary evaluation if there is suspicion of a mental illness, leading to either refusal or incapacity to acknowledge the necessity of examination. In addition, two conditions must be met: firstly, the person’s inability to self-care, risking significant harm without intervention, and secondly, the likelihood, based on recent behavior, that without treatment, they will pose a danger to themselves or others.
The Baker Act process and criteria can lead to a short-term stay at an inpatient psychiatric care facility, aiming to ensure safety while respecting the individual’s rights and balancing the need for mental health crisis intervention services with the necessity of protecting civil liberties.

Who Pays for the Baker Act in Florida?
When someone is placed under the Baker Act in Florida, the costs associated with their evaluation and treatment can be payed for by various sources. Typically, if the individual has health insurance, whether private or through government programs like Medicaid or Medicare, these plans will cover some or all the expenses.
Some psychiatric hospitals and mental health clinics may have programs to assist with mental health therapy costs for uninsured patients. It’s essential to communicate with the facility to understand the financial aspects and explore all available coverage resources. The patient is usually responsible for covering the hospital bill for involuntary placement under the Baker Act. However, the Department of Health and Rehabilitative Services (HRS) must provide treatment at a receiving facility if the patient is indigent. HRS ensures that indigent Baker Act patients receive the necessary treatment without cost to the county. Contact us for more information regarding evaluation and mental health treatment costs under the Baker Act.
Does Insurance Cover the Baker Act?
When someone is placed under the Baker Act in Florida, health insurance can often cover the costs associated with their evaluation and treatment. Most private health insurance plans, as well as government programs like Medicaid and Medicare, include coverage for mental health services, which can encompass involuntary psychiatric evaluations and subsequent care.
At our Mental Health Treatment Center in Florida, many clients frequently ask, “does insurance cover the Baker Act?” Our dedicated team is experienced in managing Baker Act Florida cases, ensuring that every inquiry about whether insurance coverage the Baker Act is met with clear, compassionate guidance. We remain committed to providing accurate support and information regarding Baker Act Florida procedures, so you can confidently navigate your mental health insurance options. Call 877-958-9212 to confirm your mental health insurance coverage today.

Baker Act Mental Health Treatment Inquires at SBHMC
Are you ready to take the first step towards better mental health? At The Sylvia Brafman Mental Health Treatment Center in Fort Lauderdale, Florida, our dedicated team is here to guide you. We offer a range of therapy programs and rehab treatments tailored to your needs – whether you’re asking, “Does insurance cover the Baker Act” or seeking support as a baker act patient in Florida. Our success stories speak volumes about our expertise and commitment. Don’t wait—call us or fill out the form below for a callback.
"*" indicates required fields

How to Baker Act Someone in Florida
To initiate a Baker Act in Florida, start by identifying if the individual poses a danger to themselves or others due to a mental illness or is unable to care for their basic needs. If the situation is urgent, contact psychiatric emergency services, as they can transport the individual to a receiving facility for evaluation.
Once the individual is at the facility, a qualified mental health professional will conduct an assessment to determine if they meet the criteria for involuntary admission under the Baker Act. If the requirements are met, the person can be held for up to 72 hours for further evaluation and treatment. During this time, mental health professionals will decide the appropriate course of action, which may include continued treatment or discharge with follow-up care. For detailed answers to the common question: How do you Baker Act a person? Call 877-958-9212.

What is a 72-Hour Hold in Florida?
In Florida, a 72-hour hold refers to the period during which an individual can be involuntarily held in a mental health facility for evaluation under the Baker Act. This temporary detention allows mental health professionals to assess the person’s condition, determine the need for treatment, and ensure their safety and the safety of others.
During this time, the individual will receive a thorough examination to identify any mental health issues and the appropriate course of action. Understanding the 72-hour hold is essential for anyone facing a mental health crisis or concerned about a loved one. This hold is designed to provide immediate intervention and support while protecting the individual’s rights. If, at any point during the 72-hour emergency mental health assessment, it is determined that the patient is not a threat to themselves or others, they must be released. After the evaluation, a decision will be made regarding the need for further treatment, which may involve voluntary admission, continued involuntary treatment, or discharge with follow-up care and support.
Contact us for additional information on The Sylvia Brafman Mental Health Center’s psychiatric day programs in South Florida.
Other Laws Similar to Involuntary Psychiatric Evaluation and Treatment
In addition to Florida’s Baker Act, many other states have laws that allow for involuntary psychiatric evaluation and treatment to ensure timely and adequate mental health crisis response. For example, California has the Lanterman-Petris-Short (LPS) Act, which permits the involuntary detention of individuals who are gravely disabled or pose a danger to themselves or others due to a mental disorder.
Similarly, New York’s Mental Hygiene Law includes provisions for psychiatric emergency intervention and involuntary commitments for psychiatric evaluation. In Texas, the Health and Safety Code Chapter 573 outlines procedures for emergency detention of individuals with mental illness. These laws vary from state to state but generally share common goals: protecting individuals in crisis, ensuring public safety, and providing timely psychiatric crisis interventions.
Statistics indicate that involuntary commitment laws are critical; for instance, the National Alliance on Mental Illness (NAMI) reported that in 2021, 5.5% of American adults experienced serious mental illness, affecting approximately 14.1 million people. This means that 1 in 20 adults faced significant mental health challenges, highlighting the need for such protective measures. Understanding these laws helps ensure that you or someone you love receives the care needed while upholding your civil liberties.

How to Find a Psychiatric Evaluation and Treatment Center in Florida
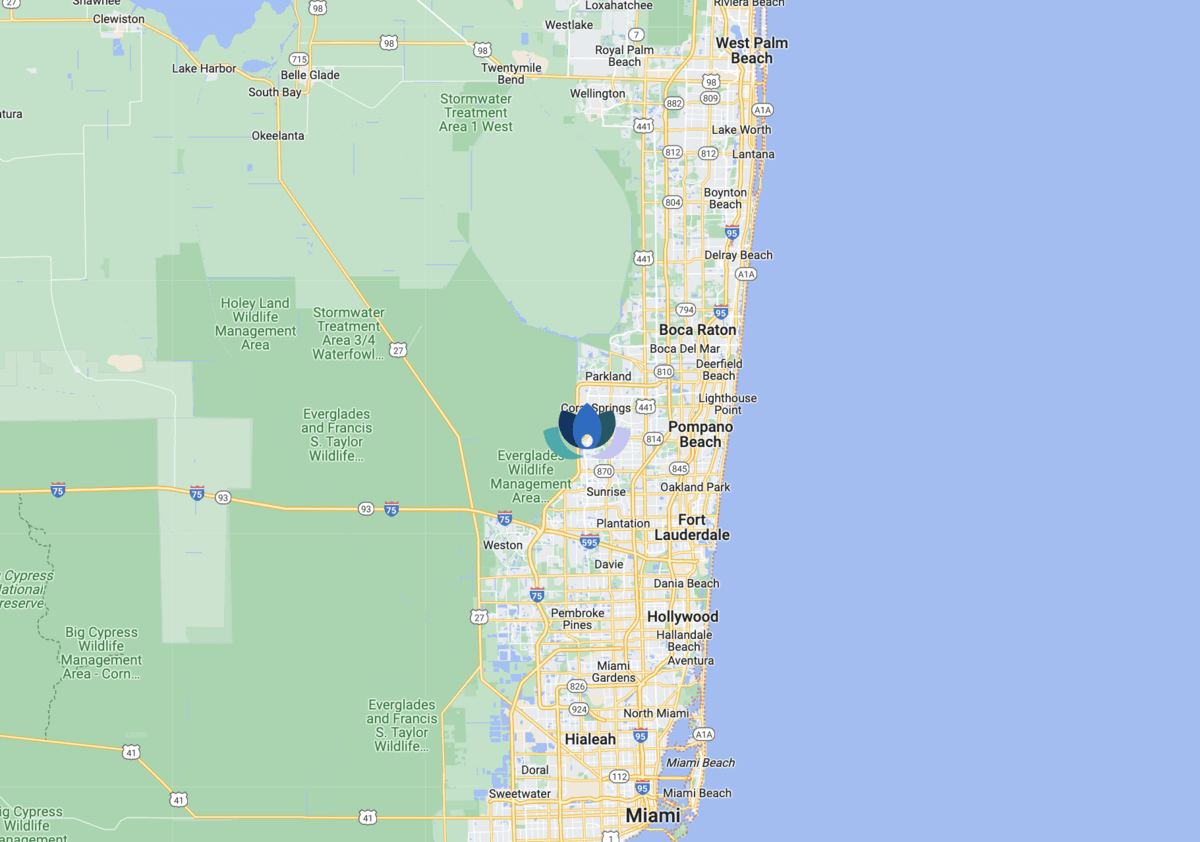
If you’re seeking psychiatric treatment centers, there are options to find the care you need. The Sylvia Brafman Mental Health Center at 7710 NW 71st Ct, Tamarac, Florida, 33321, is accredited and renowned for its dedication to evidence-based mental health programs for adults. Call 877-958-9212 for your free mental health assessment to determine the most suitable level of care for your needs.
You can also consider the following steps when searching for Baker Act mental health evaluations and behavioral health centers in the Sunshine State:
What Happens at an Involuntary Psychiatric Mental Health Treatment Facility?
At an involuntary psychiatric treatment facility, individuals receive comprehensive care and support to address mental health needs. Upon admission, baker act patients would undergo assessments by qualified mental health professionals to determine your treatment plan. Treatment typically includes a combination of therapy, medication management, and other therapeutic interventions tailored to your specific condition and needs.
In addition to clinical care, you may participate in group therapy sessions, recreational activities, and educational programs to promote healing and recovery. Throughout your stay, staff closely monitor you to ensure your safety and well-being while working toward achieving your treatment goals.



